What about my cholesterol?
Sep 29, 2021So, this blog aims to answer a question we often get asked. Doctor, what about my cholesterol?
Now a disclaimer, this is not individual medical advice. Please discuss anything you hear or read from Real Life Medicine with your treating medical practitioner.
Let’s start with the terminology.
A lipid profile is an overarching term, and it includes cholesterol, which are sterols, and triglycerides, which have glycerols.
Triglycerides
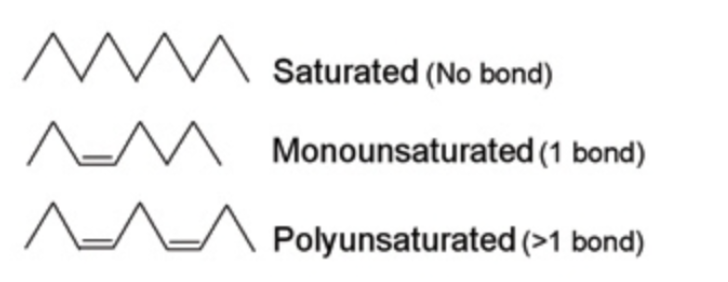
There are chains of hydrocarbons called fatty acids, and a triglyceride has three chains of fatty acids, combined with a glycerol molecule. The fatty acid chains on the triglycerides can be saturated or unsaturated. Simply put, saturated fats have single bonds between all the hydrocarbons in their fatty acids. Unsaturated fats have one or more double bonds between the hydrocarbons in their fatty acid chains. These can also be short, medium or long chain. And you will no doubt have heard these phrases - medium chain triglyceride (MCT), or short chain fatty acids (SCFA), which are commonly talked about in gut health. They have multiple roles including being useful for fuel.
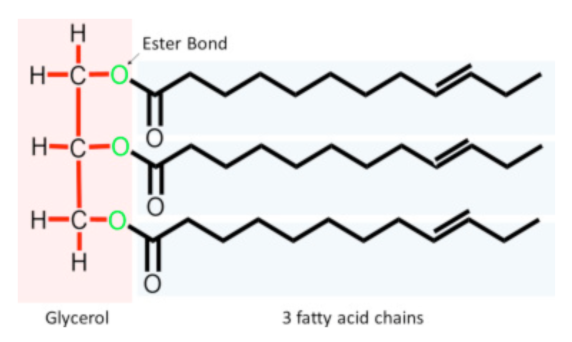
Here we have a glycerol molecule, as well as our three chains of fatty acids. Saturated fats have no double bonds, monounsaturated fats have one double bond, and polyunsaturated fats have more than one double bond. Now weirdly, you would think that the double bonds would make it more stable because it's double, but actually it doesn't. It means there's twice as many bonds to be disrupted. So in fact, polyunsaturated fats are less stable.
Dietary fat
Dietary fat is triglycerides. It can come from animals or plants. No source of fat has a single type. So what I mean is there is no pure saturated fat, nor is there pure polyunsaturated fat. All fats are a mixture of saturated, monounsaturated and polyunsaturated, just in varying percentages.
Body fat
What is body fat?
Sort of sounds obvious, doesn't it? But it's actually not that obvious.
Body fat is also known as adipose tissue. Adipose tissue is an organ and it's made up of adipocytes. Now these little adipocytes are filled with triglycerides, but that's not their only function. They can also make hormones, multiple different hormones. Some that you may be familiar with are Leptin, which is our satiety or our fullness hormone, but also Oestrogen. So when we have excessive adipocytes or excessive adipose tissue, we also make excessive oestrogen. Interesting. The other thing adipose tissue does is make inflammatory mediators called cytokines, and the special cytokines from adipose tissue are called adipokines. So when we talk about adipose tissue being inflammatory, it's because it makes these special inflammatory cells and sends them around our body. So body fat would be much clearer if we just called it adipose tissue, so we wouldn't be getting confused between this, and actual dietary fat.
What do we mean by losing weight?
We're talking about emptying the adipocytes, by mobilising the triglycerides. So emptying them, and therefore reducing the amount of adipose tissue and the activity of those adipocytes.
What is cholesterol?
Cholesterol is a type of lipid (remember our overarching term), and it's a yellow kind of waxy molecule found in all animal cells. Every single cell has cholesterol in it. And it's also an organic molecule, much like fatty acids, made up of carbon, hydrogen and oxygen. But here's the thing, we can't use it as fuel.
So why is it so important? Well, it is required to form cell membranes in every single cell of the body. It also forms myelin sheaths. Myelin is like the insulation around our nerve cells and brain cells; it is absolutely critical. And you cannot make myelin without cholesterol. It is also one of the building blocks of vitamin D. You cannot make vitamin D without cholesterol. It is also an integral component of our sex hormones. So both testosterone and oestrogen cannot be made without cholesterol. Finally, it’s also in our bile acids, which then form part of the loop that closes the recycling of cholesterol.
How do we get cholesterol?
Well, amazingly we actually make most of it ourselves. Aren't we clever? In the powerhouse, the liver, which as you know is my favourite organ. We can also ingest it from our food, where it is found only in animal food. Now, what happens to our cholesterol on a low carb diet? Well, it will often go up, not for everybody, but for some people. And the reason for this is twofold. One, we are often ingesting more of it in our food, as we are eating more eggs, dairy, meat, etc. But for some people, their liver may make more.
So what's the big deal?
Obviously we're worried about cardiovascular disease because that's what everyone associates cholesterol with. And we have this image that cholesterol forms these plaques blocking off our arteries. But high cholesterol is not an emergency. It doesn't clog up your arteries like a blocked drain. Cardiovascular disease is a prolonged process taking many, many years to occur.
But what I want to emphasise with cardiovascular disease, is that there is no single cause. We look at all sorts of things, including:
- Family history;
- Smoking history;
- High blood pressure;
- Type 2 diabetes;
- Metabolic syndrome, which is the precursor to type 2 diabetes;
- Stress;
- Inflammation; and
- Maybe cholesterol.
So we spend an inordinate amount of time focusing on one thing - cholesterol, whilst often not focusing at all on any of these other causes.
What about good and bad cholesterol?
Well the first thing is, there is no good and bad cholesterol. Cholesterol is just cholesterol, it doesn't change.
Cholesterol can’t float around in our body because it's not water soluble. So it is packaged up in something called a lipo-protein. Now the lipo-proteins carry a little bit of protein, some cholesterol, and triglyceride. They all go together like passengers on a bus, all friendly, floating around our body to be used for their various functions. It's the lipo-proteins that people have categorised to be good or bad.
Lipo-proteins
Lipo-proteins are made in our liver and they start off as something called a VLDL, very low density lipo-protein. It's a big molecule, with lots of triglycerides in it, and a little bit of cholesterol. As it moves around the body like a bus, it empties its passengers of triglycerides. It then becomes an intermediate density lipo-protein (IDL). And finally after emptying the triglycerides further, it becomes what's called a low density lipo-protein (LDL).
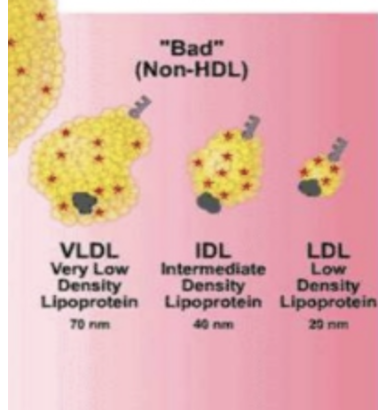
We also have a completely separate molecule, called an HDL (High density lipo-protein). Now it's these LDLs that people will refer to as the bad cholesterol, and the HDLs that people refer to as the good cholesterol. The reason HDL is called the good cholesterol is that the higher your HDL is, the lower your cardiovascular risk.
Are all LDLs bad?
The answer is no. There are 7 subtypes of LDL, named very conveniently LDL-1, 2, 3, 4, 5, 6, and 7.
We can look at something called LDL-1 and 2, and these are larger types of LDL. They are referred to as large, buoyant, or big and fluffy, and they seem to have no association with atherosclerosis or plaque formation. A lipid profile with mainly LDL-1 and LDL-2 is called Pattern A.
A profile with mainly LDL-3 to LDL-7 is called Pattern B, and is associated with cardiovascular disease. LDL-3 to LDL-7 are referred to as small dense LDL. What happens is that the protein part of the lipo-protein is damaged. The protein part of an LDL is called Apo-B100. When it’s damaged, the LDL molecule shrinks a little bit.
Damaged LDL is the small dense harmful LDL.
What causes damage to the Apo-B100 protein?
There are some people that sadly have genetic lipid disorders, but by far and away the biggest cause is actually glucose. Glucose likes to attach itself to various proteins, and it can attach itself to the protein part of the lipo-protein in a process called glycosylation. When that happens, the molecule is far more likely to oxidise, which means it's damaged. Other things that cause damage include:
- Smoking;
- Inflammation; and
- Chronic stress.
These are all associated with increased risk of cardiovascular disease.
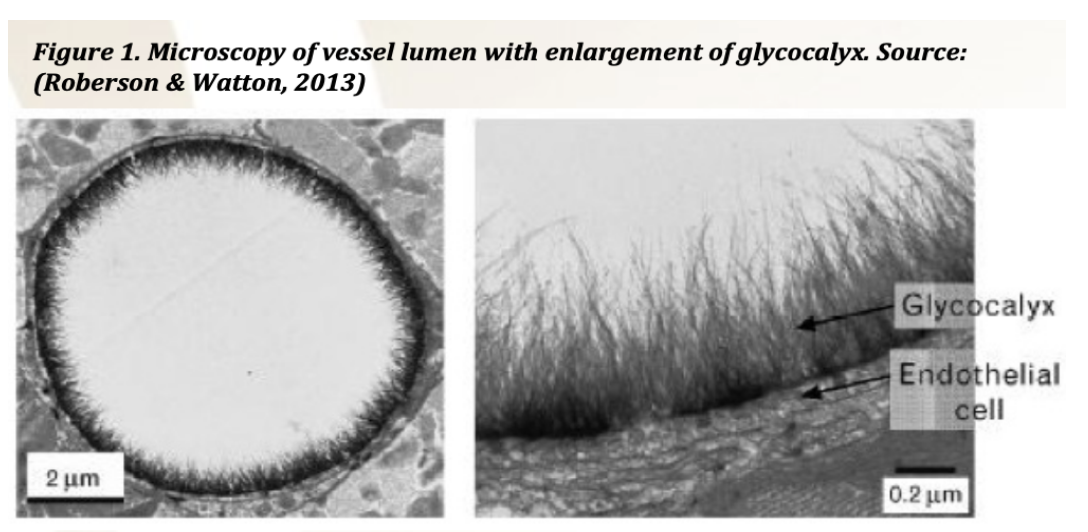
How is plaque formed?
It is a complicated process. This is a very fancy electron micrograph of the inside of a blood vessel. The inside of each of our blood vessels is protected by something called the glycocalyx. So there are several things that can damage the glycocalyx. We know that glucose can. Hyperglycemia is the number one cause of damage to vessels along with smoking. These in combination are really damaging. And then there may be the actual LDLs, the small dense LDLs that find their way in here. Remember, there's a damaged receptor in the protein of the LDL. Our body recognises that the receptor is damaged and wants to take this LDL molecule out of circulation. We have an immune process that does this. The immune cells live in the blood vessel walls, and they recognise this damaged receptor, and they actually engulf it.
It makes sense. The way I think about it, it's a bit like the sirens of the sea enticing the sailors in.
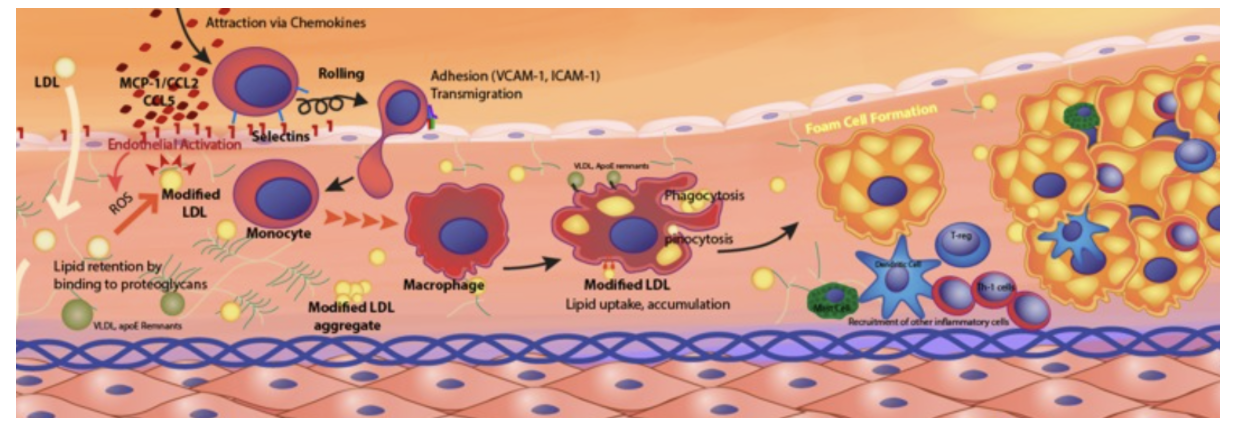
In this fancy picture, we have the LDL (small pale yellow dots on the left). It's getting enticed in through the glycocalyx (flat calls with a purple dot). We have the macrophage (immune cell) engulfing the LDLs. Munching it all up, spitting out the components, largely cholesterol, and forming these fancy things called foam cells, which all gather together, coalesce, and form a plaque within those endothelial cells (the lining of your artery wall).
Let's talk about blood tests.
When you go and have your cholesterol checked, there are three things that can be determined from your blood:
- Total cholesterol;
- Triglycerides; and
- HDL.
Now LDL is not actually measured, it's calculated. It’s worked out by putting it through a mathematical formula. So it's a very good guesstimate, but we do not actually measure your LDL in a standard lipid profile.
LDL subfraction
What you can have though is a special LDL test called an LDL subfraction.
It will measure your actual LDL, and all the subfractions. It's not covered by Medicare, and costs approximately $200 in Australia.
This test will tell you if you have the harmful type of LDL (small dense), or the unharmful type (large buoyant).
Cardiovascular disease prevention
Now where does cholesterol fit in in the prevention of cardiovascular disease?
So, we've got two things that we're looking at.
We have primary prevention, which relates to somebody who's never had any cardiovascular disease.
And we've got secondary prevention. This refers to somebody who has had a cardiovascular event.
With both of these groups, we still look enormously at lifestyle.
So:
- Smoking;
- Hypertension;
- Type 2 diabetes;
- Metabolic syndrome;
- Stress management; and
- Movement.
These factors are incredibly important in both groups.
How do you know if you've got cardiovascular disease? Well, there's some obvious ones. So if you've had a heart attack, angina, a TIA or what's called a mini stroke, a big stroke, or if you’ve got something called peripheral vascular disease, then you have cardiovascular disease and you move into the secondary prevention group.
If you haven't had any of these, well, you still might actually have some cardiovascular disease, but you just don't know it. And one of the ways that we can tell, is to do something called a Coronary Artery Calcium Score. It’s a CT scan and it gives you a score. And that score will be somewhere between 0 and 1000. So what it does is actually measure the amount of calcium in your coronary arteries.
Remember those plaques that I showed you earlier, where the macrophage is going in and munching up all the LDL and depositing the cholesterol in the walls? When it's been there for a while, they become hardened or calcified. So if you have any calcium in your arteries, then basically you have cardiovascular disease.
So if you have a score of zero, that's very reassuring.
A score under 100 is actually dependent on your age. So you may have a score of three or four, but if you are only 40, then that's quite concerning. If you have a score of three or four, but you're 65, it's much less concerning. If you have a score of 50 and you're 50, again, concerning. If you have a score of 50, but you're 80 years old, not so concerning.
So these numbers are really age dependent and require interpretation. A score over 100 really indicates significant underlying cardiovascular disease. And if the calcium score is done properly, it will be able to tell you which arteries this plaque is deposited in. So this is the $64,000 question.
What about cholesterol medication?
Should I take a statin?
So this is my approach. Remembering this is not individualised medical advice, but this is an approach that I like to use. I'll do a full assessment. And the full assessment of the risk includes family history, smoking status, and insulin/glucose. I ask about stress management, and their inflammatory state. Do they have underlying cardiac autoimmune conditions? Do they have cancer? Have they got active or low grade chronic infections? All of these increase your inflammatory risk, damaging the glycocalyx and the Apo-B protein on the LDL. I will also assess obesity because of the nature of those pesky adipocytes. I will often do an LDL subfraction, and I'll do a coronary artery calcium score.
Risks vs Benefits
I discuss the risks of cholesterol medications. Overall, they're a pretty safe medication. Some of the medications that we use in medicine are not very safe. Anti-inflammatory medications for example, even though they're very prevalent and you can buy them in the supermarket, come with a significant risk of bleeding disorders, gastric ulcers, etc. Clearly some of our immune modulators, in things like rheumatoid arthritis and cancer, can be quite toxic and require careful monitoring. So overall statin medications are reasonably safe. However, they are a lifelong medication. And I think that needs to be taken into account. And for some people they cause significant muscle issues. This may be pain, and less commonly a serious condition called rhabdomyolysis. Other people may experience abnormal liver function. And there is emerging evidence that they may increase the risk of type 2 diabetes in susceptible people. And as we've discussed glucose in itself is a risk factor.
What about the benefits?
Well, there's certainly a lot more evidence in secondary prevention, and there is a lot more evidence in acute cardiac events, particularly if you've had a stent. We also think that part of the benefit is that they improve plaque stabilisation.
The cause of a cardiovascular event is often the rupture of one of these plaques. And then either little bits of plaque go further downstream and block smaller arteries, or you get blood coming along and clotting, trying to repair the plaque and causing a thrombosis. Again, either at the site or further downstream.
And there are some people on a low carb lifestyle who have extraordinarily high cholesterol. So these are numbers way above 10; some people end up with cholesterol of 10, 12, or 18. We don't know the implication of very high cholesterol for these people. And I think it would be folly to just assume that it's harmless because we actually don't know.
So with all discussions, you need to consider risk versus benefit.
So for example, if I saw somebody and they were looking at primary prevention.
They have no risk factors, they don't smoke, they don't have type 2 diabetes and they have normal blood pressure. Maybe they've had a calcium score of zero, and their LDL subfractions are pattern A. In this case, it is really unlikely that their cholesterol level is going to cause them a problem. The evidence of benefit in this case is not very strong.
What about somebody who comes in with secondary prevention? So they've had a cardiovascular event. They have some underlying risk factors. They've got a calcium score that's above 100, and their LDL subfraction is pattern B. The evidence of benefit for them is much stronger, combined of course, with modifying the other risk factors.
So I think in summary that a proper discussion, including a risk benefit analysis for each individual, really needs to take place. There are no drugs that are without side effects, but sometimes despite our best efforts disease does occur, and we may have something that can help.

